Toenail fungus can be difficult to treat, and cold laser is emerging as a promising additional therapy.
Onychomycosis – What Is It?
Onychomycosis is a fungal infection of the toenails (more common) and fingernails (less common) caused by dermatophytes, nondermatophyte molds (NDMs) and yeasts. Dermatophytes cause 60-70% of cases, followed by NDMs (30-40%), and then yeasts (10-20%).1 The most common offending organism is a dermatophyte called Trichophyton rubrum, and other culprits include Trichophyton, Epidermophyton floccosum, Microsporum spp., Trichophyton violaceum, to name a few. It is now becoming clear that nail fungal infections can be caused by 2 or more organisms. Another important discovery is that these critters often form biofilms, which helps to protect them from antifungal drugs, to evade the host’s immune system, and to serve as a source for persistent infection2. This is a big reason why these infections can be difficult to treat.
What are the symptoms of nail fungus?
Fungal infection of the nails causes unsightly color changes in the nail. Typically there will be yellowing or browning of the nail, but certain types of fungal infections can cause purple or even black discoloration.1 The nail often becomes thickened and brittle, and there may even be hyperkeratosis underneath the nail, leading to onycholysis – or separation of the nail from the skin. A big problem with nail fungal infection is the negative psychosocial impact this has on a person’s quality of life3. In addition, these infections can cause pain and discomfort. Toenail fungus infections are typically accompanied by Tinea pedis, or athlete’s foot infections. In fact, there are just a few instances when onychomycosis will occur on its own. This can happen if someone uses contaminated nail clippers or via direct fungal inoculation into the nail during a pedicure.4
Who is Affected?
Nail fungal infections are more common in adults than children and more common in men than women. The US prevalence is estimated to be 13.8% in adults, and in people over 70 years of age, this may increase to up to 50%.5 Other at-risk populations include diabetics, people with poor peripheral circulation, and people who are immunosuppressed. In people with these comorbid conditions, treatment is particularly important to avoid spreading infection, including complications like cellulitis.
What are other risk factors for nail fungal infections?
Risk factors for onychomycosis include trauma to the nail, advancing age, athlete’s foot, psoriasis, diabetes, malignancies, and immunosuppression. There appears to be a genetic susceptibility as well with an increased prevalence in people with the HLA-DR8 serotype.1
What Are the Treatments for Nail Fungus?
The most common treatments for nail fungus are oral and topical antifungal treatments. Oral treatments are preferred for more severe infections because they can penetrate the nail bed and nail plate. However, they can also cause side effects like headache, digestive symptoms, nausea, and even hepatotoxicity. In addition, there can be drug-drug interactions, so oral antifungals may not be suitable for people already taking multiple other drugs6. Terbinafine and itraconazole taken daily for 3 months are the oral treatments approved for this condition, and their complete cure rates are only 38% and 14%, respectively4.
Topical antifungal treatments have the benefit of being safer and avoiding drug interactions, but the downside is that they have also been less effective and require a very long treatment time. In the past, topical treatment has been recommended mainly for mild cases; however, efinaconazole 10% solution was studied in mild and moderately severe cases with daily application for 48 weeks and then further follow up until week 52. Mycologic cure was obtained in 53-55% and total cure in 15-18%5.
Diagnosis and cure in onychomycosis
When nails are colored, brittle and thickened they are called dystrophic. While onychomycosis is the main reason for dystrophic nails, it is not the only one. Therefore, it is recommended that confirmatory testing is done before treating nail fungus. This can be done with microscopy (evaluating a tissue sample under a microscope after it has been treated with potassium hydroxide), fungal culture, or PCR testing.
After treatment, there are two ways of evaluating “cure”. Mycologic cure is when microscopy and fungal culture are both negative, indicating that the fungal infection is no longer present. Clinical cure has to do with the appearance of the nail and requires time for the nail to grow out. Complete cure occurs when mycologic testing is negative and the toenail is clear. It is possible to have both or one or the other. Clinical cure can take a year or more depending on what part of the nail is affected because nail growth occurs slowly at roughly 1mm per month.
Laser as alternative treatment for nail fungus
Because nail fungus is notoriously difficult to treat with neither oral nor topical treatments being ideal, there is a need for alternative approaches. Laser therapies using a variety of different wavelengths have been studied and present a promising alternative or complementary treatment. The 1064-nm Nd: YAG lasers are commonly used to treat onychomycosis, and studies have shown mixed clearance rates between 51-100%7. It is thought that this wavelength can kill fungus through its thermal effect. While overall this is a safe treatment, because the fungicidal effect occurs through heat, there can be some pain experienced with this procedure.
A retrospective study was done looking at the effectiveness of using a non-thermal, low-level laser in treating mild, moderate, and severe toenail fungus. The study analyzed the results from 3 nonrandomized, open-label studies that used a laser device combining 405nm and 635nm wavelengths8. The rationale with these wavelengths is that the 405nm spectrum is antimicrobial, and the 635nm spectrum is anti-inflammatory and promotes improved peripheral blood circulation.9 The studies used weekly 12-minute treatment sessions for either 2 or 4 weeks. The subjects of the study were not allowed to take or engage in any other treatment for toenail fungus beside the laser treatment. The goal of the study was to see if there was at least 3mm of clear nail growth over a 6-month period after the last treatment. Study treatment success was defined as at least 60% of treated toenails meeting minimum of 3mm of clear toenail growth. The results were that 67% of treated toenails met this 3mm minimum of clear toenail growth at 6 months. 89% of treated toenails had an increase in clear nail growth, and 11% had a decrease in nail clearing.
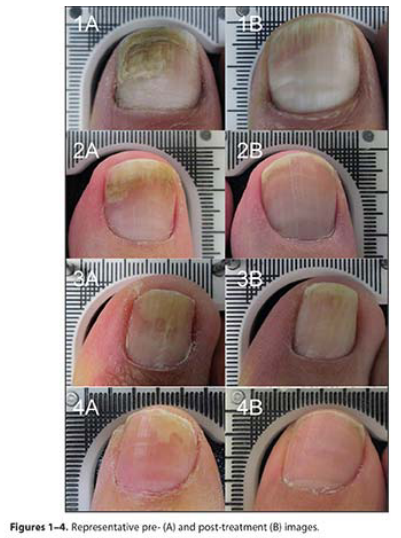
There were no adverse reactions to the treatment. Although this was not a randomized, double-blind, controlled study, which is considered high-level evidence, these results are still impressive, considering how safe, comfortable and minimally invasive the treatment is. An Irish podiatrist named Robert Sullivan, MSc, was originally skeptical when he learned about this cold laser treatment for onychomycosis, but he went on to document the effects of low-level laser on 800 toes with onychomycosis over an 18-month period and found and 89% treatment success rate.8
Fungal nail infections can cause psychosocial stress and reduction of quality of life. Treating these infections is important because they are contagious, and persistent infections can serve as reservoirs for other fungal infections in the body. This is particularly a concern in people with diabetes, the elderly, and the immunocompromised. However, typical treatments can be painful or have unpleasant and even dangerous side effects. Therefore, topical treatments like efinaconazole 10% solution and cold laser present attractive options that are both safe and effective.
Featured image: Content Providers(s): CDC/Dr. Edwin P. Ewing, Jr. Creation Date: 1997
REFERENCES:
1. Lipner SR, Scher RK. Onychomycosis: Clinical overview and diagnosis. J Am Acad Dermatol. 2019;80(4):835-851. doi:10.1016/j.jaad.2018.03.062
2. Gupta AK, Daigle D, Carviel JL. The role of biofilms in onychomycosis. J Am Acad Dermatol. 2016;74(6):1241-1246. doi:10.1016/j.jaad.2016.01.008
3. Gupta AK, Mays RR. The Impact of Onychomycosis on Quality of Life: A Systematic Review of the Available Literature. Ski Appendage Disord. 2018;4(4):208-216. doi:10.1159/000485632
4. Rich P, Health O, Tosti A, Scher R. Onchomycosis: an overview. 2013;(July 2016).
5. Rodriguez DA. Efinaconazole topical solution, 10%, for the treatment of mild and moderate toenail onychomycosis. J Clin Aesthet Dermatol. 2015;8(6):24-29.
6. Christenson JK, Peterson GM, Naunton M, et al. Challenges and opportunities in the management of onychomycosis. J Fungi. 2018;4(3). doi:10.3390/jof4030087
7. Bhatta AK, Keyal U, Wang X, Gellén E. A review of the mechanism of action of lasers and photodynamic therapy for onychomycosis. Lasers Med Sci. 2017;32(2):469-474. doi:10.1007/s10103-016-2110-9
8. Zang K, Sullivan R, Shanks S. A retrospective study of non-Thermal laser therapy for the treatment of toenail onychomycosis. J Clin Aesthet Dermatol. 2017;10(5):24-30.
9. Tumolo BJ. Clearing Onychomycosis through Low-Level Laser Therapy. Pod Manag. 2017;(January):2-4.